The University of Illinois Urbana-Champaign ended the year by surpassing a major milestone. The campus completed more than 1 million coronavirus tests during the fall term to the tune of roughly $4 million a month.
The university screened students at least twice a week, administering around 10,000 tests each weekday and slowing that pace during the weekends. A campus lab worked nearly around the clock to process them, enabling students to receive their results within five to 10 hours.
The aggressive testing policy appears to be paying off. The share of coronavirus tests that returned positive peaked at 2.9% in late August, right after in-person classes began, and stayed mostly under 1% for the rest of the term, according to the university's coronavirus dashboard.
Approaches to coronavirus testing varied widely among colleges in the fall, with schools selecting methods based on their enrollment, budgets and access to lab facilities. While UIUC has one of the most aggressive testing strategies in the nation, not all colleges have the funds or capability to provide such extensive screening.
The University of Denver, a private research institution enrolling around 12,000 students, conserved resources in part by monitoring wastewater to pinpoint virus outbreaks. And Syracuse University, which has about twice as many students, used pooled testing, in which several samples are screened together and analyzed individually only if the batch turns up positive.
"Intensive testing is expensive," said Heather Pierce, senior director for science policy and regulatory counsel at the Association of American Medical Colleges. "Schools that are looking to reopen or stay open are trying to figure out the best use of their resources to monitor for the virus."
1 million tests and counting
Before the fall term started, UIUC officials knew they wanted to test students twice weekly for the coronavirus. One study published this summer indicated this level of testing was necessary to control outbreaks, and the AAMC recently recommended regular testing to safely reopen schools and universities.
However, colleges that can't process thousands of tests in their own facilities will have to outsource this work. That may be untenable for local labs already overwhelmed with the testing needs of their communities. Schools may also have to make trade-offs between highly accurate tests that must be processed in a lab and ones that miss more cases but are less expensive and can be administered on-site, Pierce said.
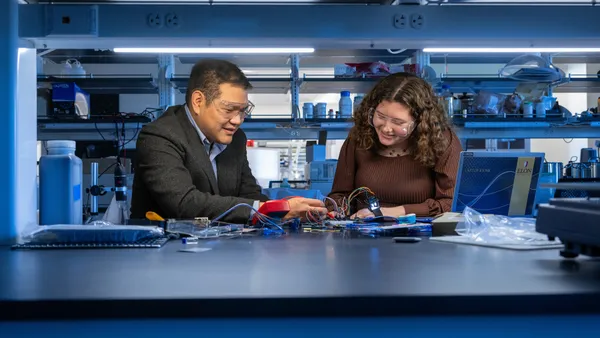
At the UIUC, which enrolls more than 50,000 students, Paul Hergenrother led a team that developed a saliva-based test that could be processed quickly through the university's labs and wasn't as invasive as nasal swabs. Hergenrother, a chemistry professor at the university, said it detects the coronavirus two to three days sooner than some other widely used tests.
The tests are key to the university's plan to prevent the coronavirus from spreading. Students and employees gain access to campus buildings by presenting their negative test results on a mobile app, which alerts them when they need to be screened again. They can get a coronavirus test at about 20 campus locations, where completed tests are picked up and taken to the lab hourly.
UIUC hired more than 200 workers for its testing efforts. "It's a massive operation," Hergenrother said. It cost around $6 million to $7 million to establish the testing system, a chemistry trade publication reported in November.
Although the fall ran smoothly, officials are polishing their approach for the spring. They'll be testing some student groups three times a week depending on their risk factors for infection, such as whether they frequent gyms or take public transportation, Hergenrother said.
A new kind of early-alert system
The University of Denver used a multi-pronged approach to target who they screened in the fall. One component was monitoring residence halls' wastewater for the coronavirus.
Corinne Lengsfeld, U of Denver's senior vice provost for research and graduate education, said a small team collected wastewater samples three times a week from six dorms and sent them to an off-site company for analysis. Altogether, the wastewater operation is expected to cost roughly $250,000 for the academic year.
If officials detected elevated levels of the virus in a dorm's wastewater, then students living there were tested. To help blunt potential outbreaks, around a half-dozen contact tracers tracked down where they may have caught the virus and to whom it might have spread.
The university also monitored how often smaller groups, usually made up of a few dozen students, tested positive for the virus to help determine who should be tested. Those groups could be based on students' co-curricular activities or class schedules, or comprise those living in the same wing of a dorm. Several events could trigger even closer monitoring of these groups, such as if officials learn students violated campus health measures.
However, the American College Health Association advises colleges not to replace robust testing with wastewater monitoring, in part because it can't gauge how many people are infected.
Syracuse University, in New York, also monitored residence halls' wastewater during the fall term, requiring all students in a building to be tested if the virus was detected, David Larsen, a public health professor, said during a virtual conference earlier this month hosted by U of Denver.
The private research university, which enrolls around 22,000 students, paired this strategy with contact tracing and pooled screening of 12 coronavirus tests at a time, Larsen added. The Centers for Disease Control and Prevention in November suggested this type of testing as one way colleges can save resources while still quickly completing coronavirus tests.
However, it only works if infection rates are low, AAMC's Pierce said. "Otherwise, every pool is positive, and you're just doing an extra test."
Higher positivity rates could heighten the need for individual testing on campuses this spring. Coronavirus cases are surging throughout the U.S., with some hospitals treating dangerously high numbers of patients in their intensive care units.
U of Denver is one of many institutions ramping up their testing efforts for the spring quarter in response. Students in campus housing will be tested twice weekly, while other undergraduates will be tested only once per week, Lengsfeld said. Graduate students and faculty members will be screened less often.
The university is increasing the number of coronavirus tests it is administering during its winter quarter as compared to the fall, with total winter testing expected to cost around $5 million. But the university's plans could change depending on how COVID-19 rates fluctuate during the spring.
"Everybody hopes the virus will be a little less prolific," Lengsfeld said. "We might be able to back off a little bit."